Angela Howard was not expected to live past childhood. Diagnosed with sickle cell disease at age 2, her doctors and nurses predicted the painful disease would kill her by age 18. Now 52, Howard has dedicated her life to educating the public about the stigma and misunderstanding associated with sickle cell disease.
She is not alone in this fight. A new commission report from The Lancet Haematology outlines the global burden caused by sickle cell disease and identifies the need for important governmental commitments and investments. It also offers health care-related and education recommendations experts say would improve outcomes for those living with the blood disorder, which mainly occurs in the Black population.
University of Florida College of Nursing researcher Diana Wilkie, Ph.D., R.N., FAAN, the Prairieview Trust - Earl and Margo Powers Endowed Professor, is a co-author of the commission report, published July 11. The commission includes 33 co-authors comprising experts in sickle cell disease, as well as patients and activists from around the world.
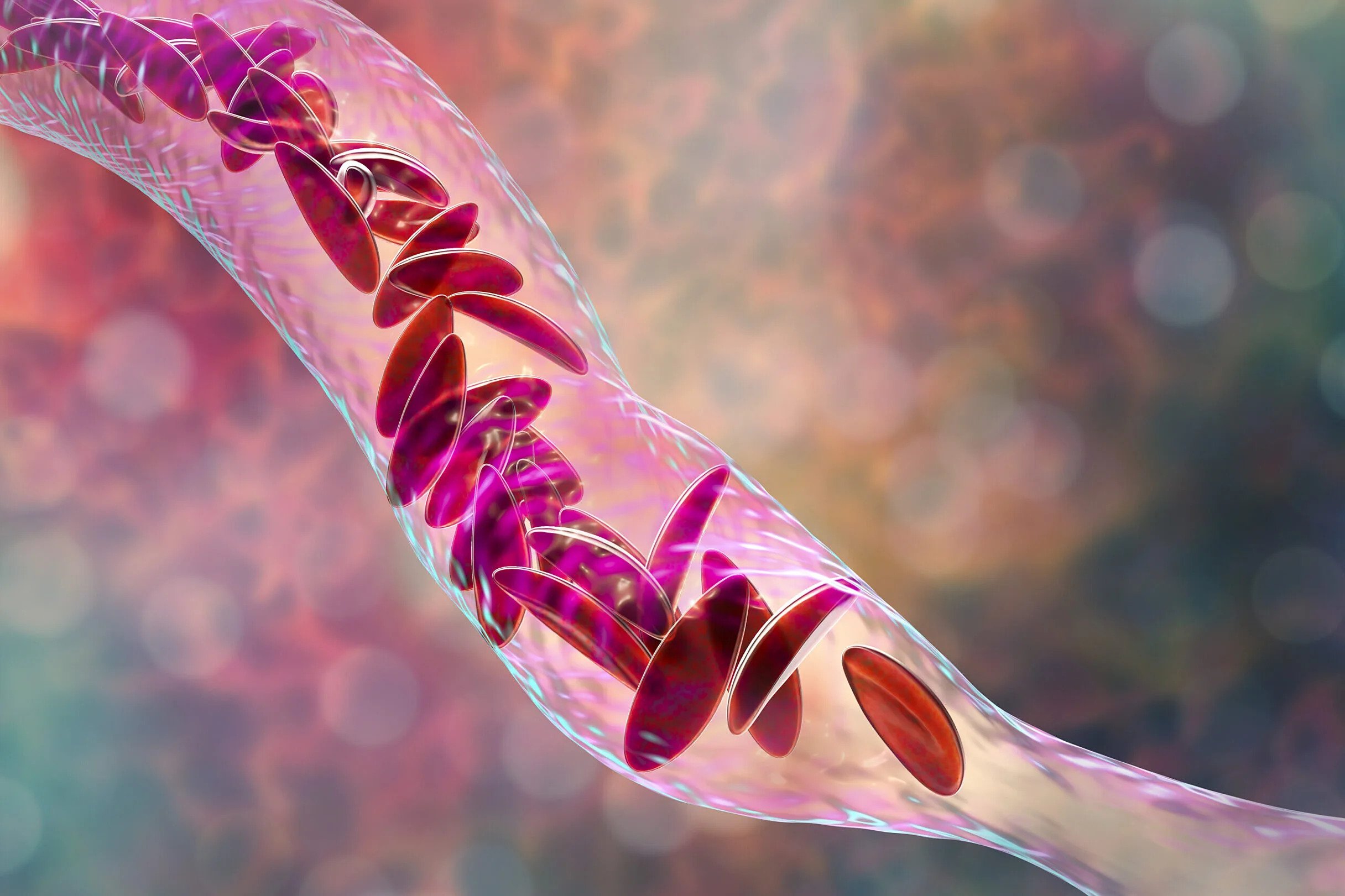
Sickle cell disease is an inherited disorder that changes red blood cells into a C shape. People with sickle cell disease report being stigmatized due to their race and because they may be seen as drug seekers or addicts when they pursue medications to control pain.
The commission reports that sickle cell disease is one of the most common severe inherited diseases in the world, and 95% of people diagnosed with it live in low-income and middle-income countries, particularly in sub-Saharan Africa and India. Although diagnosis is inconsistent, as many as 8 million people worldwide are estimated to have sickle cell disease. According to the Centers for Disease Control and Prevention, approximately 100,000 Americans are living with the condition, which occurs in about 1 out of every 365 Black or African American births.
Wilkie — an expert on sickle cell disease, health disparities and palliative care — was most involved in the education portion of the commission report. She said it is crucial for health care professionals, the public and individuals with sickle cell disease to understand its severity and how it can be better managed.
“It is critical for individuals with sickle cell disease or sickle cell trait to understand the genetic inheritance of the disease and to know about reproductive options that will allow them, if it is their wish, to avoid their child being born with sickle cell disease,” Wilkie said. “On the other hand, it is just as important for health care workers to believe people who say they are in pain and to give them appropriate therapies to control it. We need a workforce educated about sickle cell disease and committed to eliminating the stigma and health disparities of this disease.”
The Lancet Haematology Commission’s report calls for the global standardization of collecting routine epidemiological data by the year 2025 and, further, for countries to be held accountable for public health intervention measures and progress. Most people with sickle cell disease are not properly diagnosed until the onset of symptoms. Conducting mandatory newborn screenings would allow for treatment to be provided before symptoms develop.
Another recommendation involves the accessibility of effective treatment and further development of innovative treatment methods. Penicillin, the drug hydroxyurea and blood transfusions are all effective but are not available in low-income countries where sickle cell disease is prevalent. The commission implores governments to give people access to a minimum standard of health care regardless of where they live. Additionally, access to innovative treatments, like stem-cell transplantation and gene therapies, should be expanded and studies accelerated to provide safe, accessible and affordable cures globally by the year 2040.
Howard, the president of the Sickle Cell Association of North Central Florida, is a citizen scientist who encourages her community to participate in UF Health research projects to advance expertise and understanding of sickle cell disease. She also volunteers as a guest speaker for UF medical students, sharing her experience with the disease.
“When I was a child, they didn’t really know much about sickle cell,” Howard said. “It was considered an orphan disease. I’ve lived to be an adult, but I think a lot of that has to do with me becoming educated about my disease and learning the things that trigger a crisis. I’ve learned to eat healthier, stay hydrated, exercise and avoid stress.”
For furthering education, Wilkie points to the current work taking place at the College of Nursing, including her own CHOICES project — a web-based educational tool that helps young adults understand sickle cell disease and prevent it from being inherited — and self-management interventions from professor Miriam Ezenwa, Ph.D., M.S.N, R.N., FAAN, that help improve pain management.
“The work being done at the College of Nursing is an important piece to contributing to the elimination of health disparities and promoting health equity,” Wilkie said.
Wilkie said it is important to advance innovative treatments, but she is also a proponent of using palliative care principles to manage the disease and symptoms.
“This vulnerable population deserves better care than they have been receiving,” Wilkie said. “We have made progress over the years, but we still have a long way to go. I am very honored to be a part of this group of international scholars who are committed to improving the lives of people living with sickle cell disease.”
This story was originally published by the University of Florida on July 12, 2023.