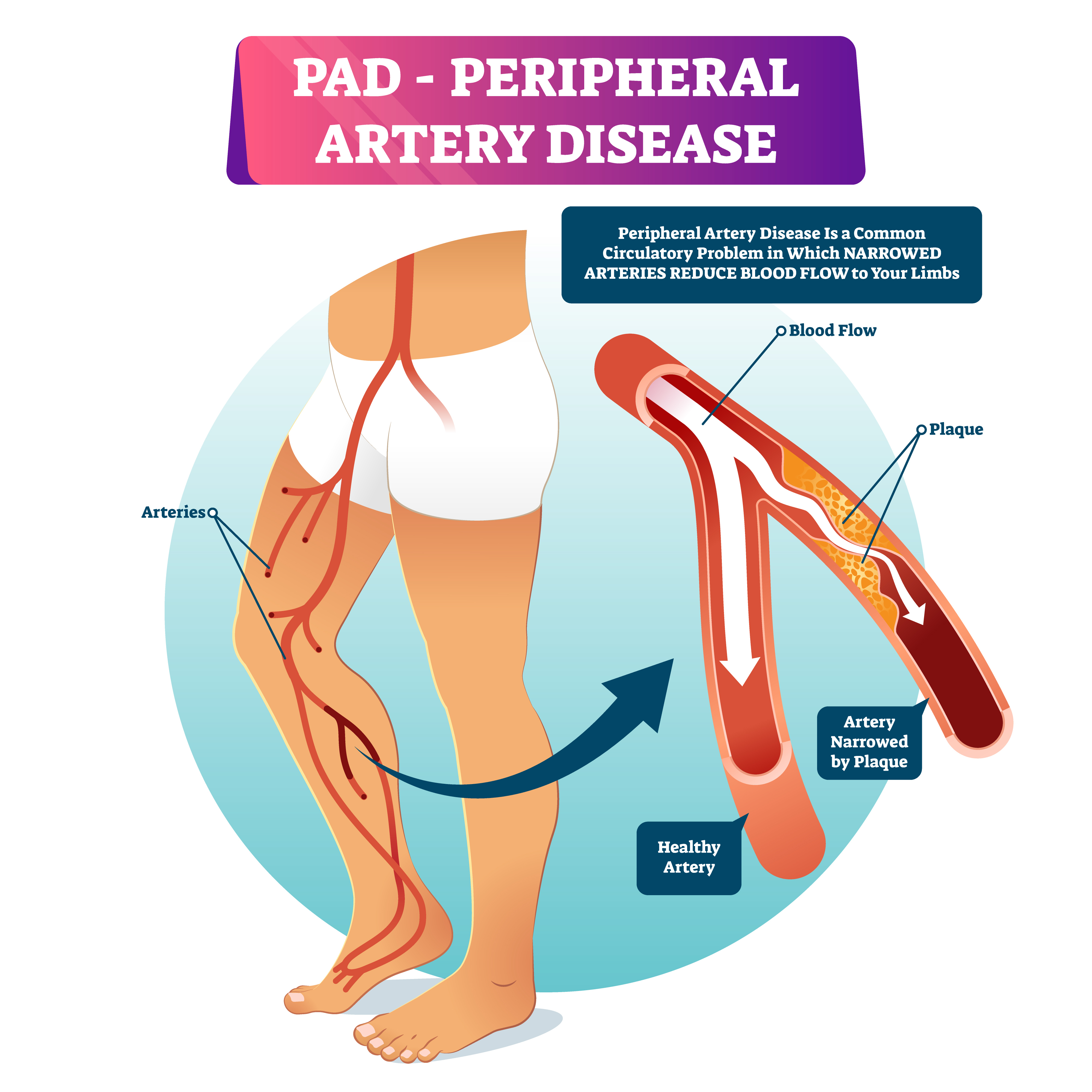
New research led by Emory Healthcare, in partnership with the Veterans Health Administration, is shining a light on the need for better medical interventions and more aggressive treatment for veterans with peripheral artery disease (PAD), a serious condition found in 10 million U.S. individuals nationwide that is one of the leading causes of the 185,000 major lower extremity amputations that happen each year.
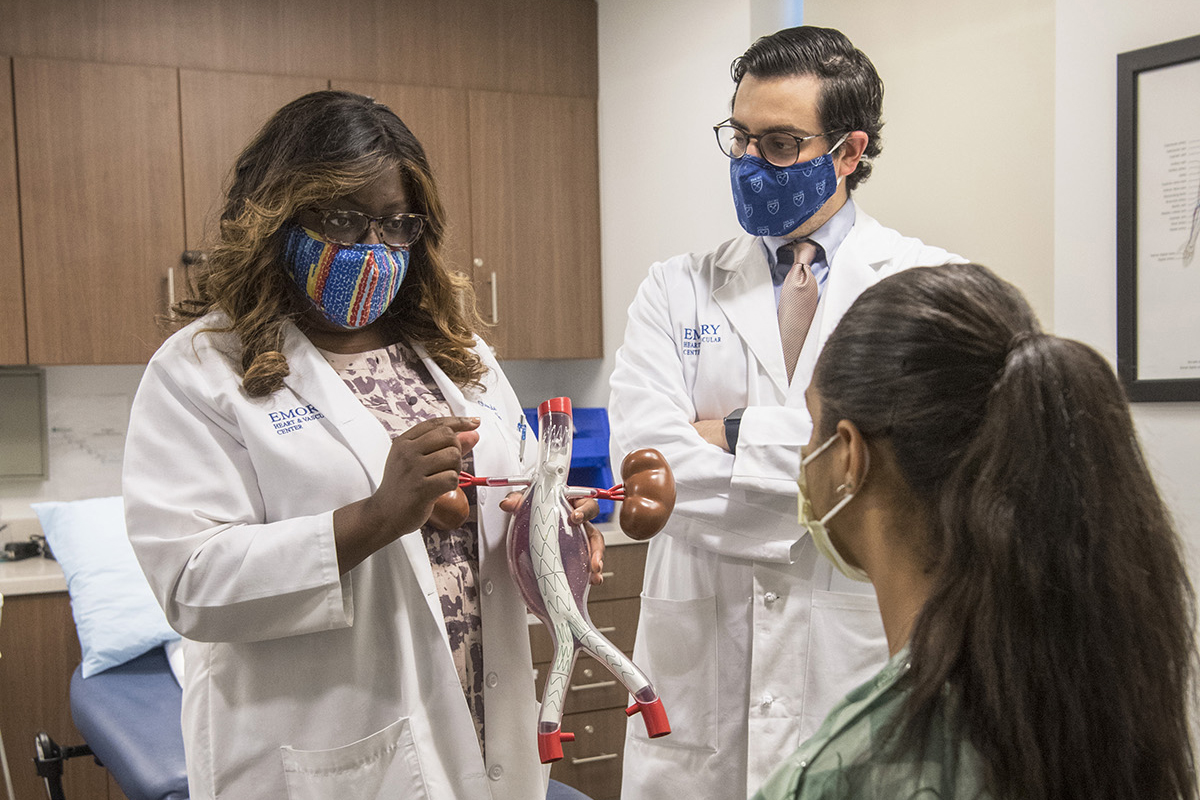
In a study published Wednesday morning in JAMA Surgery, lead author Olamide Alabi, MD, a vascular surgeon who splits her time between Emory Healthcare and the VA (Veterans Affairs) Atlanta Healthcare System, investigated ten years’ worth of health records from the U.S. Department of Veteran Health Affairs, the nation’s largest integrated health care system. To better understand what happened to the veterans who lost their limbs during the study period of 2010-20, Alabi and her team wanted to examine health care utilization in the year before amputation.
Looking closely at the varied paths taken by more than 19,000 patients who went through amputation, Alabi and her team identified several factors that impacted the quality and intensity of care these patients received prior to that major loss of limb, such as distance to primary care and geographic region.
 To that end, veterans who lived 13 miles or more from their primary care physician were less likely to receive vascular screening, a step that can potentially lead to quicker intervention. Meanwhile, veterans who resided in the Midwest were more likely to undergo vascular screening in the year prior to amputation than those who lived in other regions.
To that end, veterans who lived 13 miles or more from their primary care physician were less likely to receive vascular screening, a step that can potentially lead to quicker intervention. Meanwhile, veterans who resided in the Midwest were more likely to undergo vascular screening in the year prior to amputation than those who lived in other regions.
A diagnosis of PAD, which disproportionately impacts veterans, carries with it a myriad of significant concerns. With PAD, the risk of heart attack, stroke and death increases threefold. Also, individuals diagnosed with the most severe form of PAD have up to a 25% chance of having to have a limb amputated within one year after diagnosis.
However, limb amputation is also preventable through early diagnosis, monitoring and medical management, and subsequent revascularization (a type of medical and surgical therapy) for those who need it. The fact that patients can receive such significant variation in quality and speed of diagnostic and therapeutic care before they wind up needing amputation is what drove Alabi to give the issue a closer look at the national level.
These initial findings suggest that some veterans may be at greater risk of receiving worse care for their PAD, and that developing clinical programs, such as remote patient monitoring and management, may help.
Prior to this study, it has been unclear why some patients do or do not receive a vascular screening prior to amputation or how best to address the variables at play. One possible explanation is that many current guidelines do not recommend routine PAD screening in individuals who are asymptomatic, even though asymptomatic patients represent the largest subset of those living with PAD.
Similar research has been conducted to look at vascular interventions in the year prior to an amputation among Medicare recipients who got treatment in the private sector. In Alabi’s research, she found that veterans received vascular assessment at a higher proportion than those in the private sector.
Alabi hopes to further explore the differences between care in the private sector and care in an integrated health care system for patients with PAD, citing the fact that “some of the disparities that we see in PAD care prior to an amputation (among veterans) do not exist or do not exist to the same degree that they do in the private sector,” she said.
“There is a great deal of data suggesting that Black patients do not get vascular assessments at the same rate as white patients in the private sector,” Alabi said. “At the VHA, however, this study found that Black veterans were either more or just as likely to receive a vascular assessment in the year prior to amputation.”

Overall, Alabi believes this research is a starting point. It presents an opportunity to focus on how to establish earlier diagnosis of PAD and prompt earlier referrals to vascular specialists. An important first step toward that goal may involve identifying and highlighting best practices within high-performing hospitals or regions, which could then contribute to the creation of uniform, national guidance.
Other key points from this study:
- The data was collected prior to the pandemic.
- The vast majority (more than 98%) of veterans in this study were male and the mean age was mid-60s.
- A total of 26.6% of veterans in the study were African American or Black, 0.8% were American Indian or Alaska Native, 0.2% were Asian, 0.7% were Native Hawaiian or Pacific Islander, 65.9% were white, and 5.7% had unknown race and ethnicity.
- Individuals who identified as having Hispanic ethnicity comprised 6% of the study population, and 94% had non-Hispanic ethnicity.
- Geographically, 20.3% lived in the Midwest, 13% in the Northeast, 35.7% in the Southeast, 15% in the Southwest, and 16% in the West.
- In the year prior to amputation, 8% of this cohort study had no primary care visits and 30.1% did not have a vascular assessment.
- Nearly half of veterans in the cohort (49.9%) did not have an outpatient clinic visit with a vascular surgeon in the year prior to lower extremity amputation.
- Future research is needed to better define the reasons for regional practice variation and the role of local resource availability (such as presence of a vascular surgeon, registered vascular technologist) in the quality of veteran vascular care.
This story was originally published by Emory University on April 16, 2023.